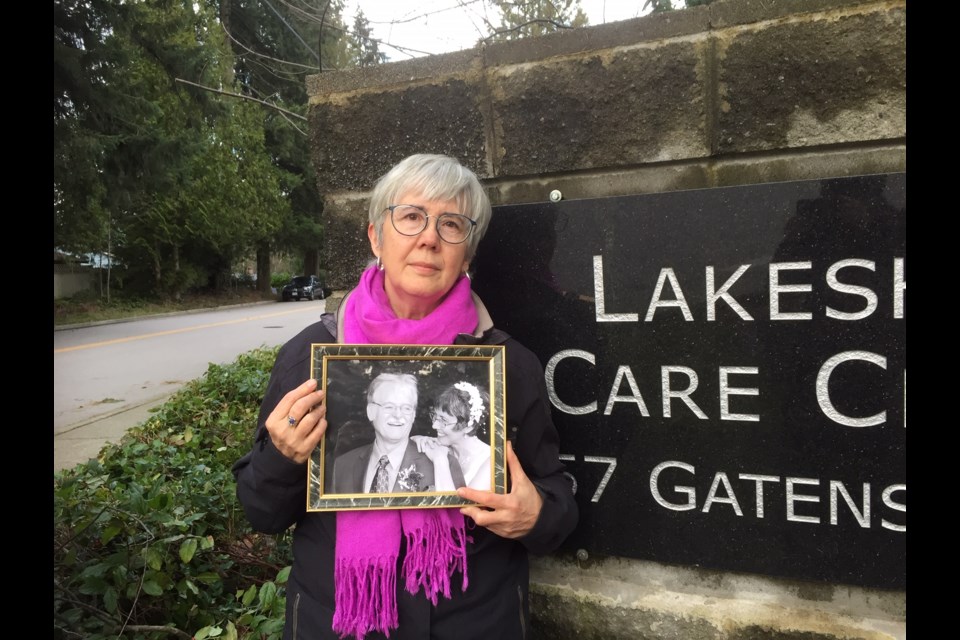
Kate Cochlan faced a difficult task this week when she picked up a bag of belongings from the Coquitlam care home where her husband passed away of COVID-19 complications.
Cochlan’s husband, Trevor Nash, died Dec. 29 at Lakeshore Care Centre, one of 21 victims of the deadly coronavirus that swept through the 56-bed facility Dec. 4 to Jan. 8.
The bag of clothing and recorders, reminders of Nash’s love of music, provide Cochlan with a tactile memory of the husband she lost — her partner, who enjoyed calligraphy, and was a BC Hydro statistician and attentive father of three before he got Alzheimer’s.
The belongings are no solace as she grieves over her husband’s recent death due to COVID-19, after seeming to rally for a few days.
Even now, Cochlan wonders about what happened and if anything could have been done differently to prevent COVID-19 from spreading so quickly through the facility.
In all, 75 people, including 43 residents and 32 staff, contracted the disease over those four weeks, leading to a 77% infection rate and a 38% death rate among all residents.
QUESTIONS REMAIN
“I think there are huge questions that have to be asked about the gaps in long-term care for it to move the way it did,” said Cochlan, who led Lakeshore’s family council.
Over the past several months, families of seniors in Tri-City care homes have chafed at restrictive visiting rights, even as asymptomatic staff were bringing in the virus, and questions have been put to provincial health officer Dr. Bonnie Henry and Health Minister Adrian Dix over why rapid testing of care home staff wasn’t introduced sooner.
Some of these concerns are being dealt with as B.C. health officials grapple with efforts to combat the deadly virus. A pilot was started in December in Vancouver Coastal and Fraser Health care homes to study whether rapid testing is effective in reducing the spread of coronavirus in long-term care facilities. And Friday, Fraser Health reported it was on track to vaccinate residents and staff at 151 long-term care and assisted living facilities by the end of the day.
But, for Cochlan, these initiatives come too late.
STAFF STRUGGLED
“It’s hard for me to hear those things, it’s tough when it’s this close to the vaccine. I told Trevor ‘just hold on, the vaccine is coming.’”
Cochlan says she sympathizes with staff who struggled to fend off the disease, many contracting it themselves.
“They are wonderful those staff. I hope they’ve all come through it OK. That’s the part you don’t hear much about.”
However, she wonders why rapid testing wasn’t done sooner in the care home sector if it was seen as useful by professional sports teams and the film industry, and Cochlan said she supports B.C. senior advocate Isobel Mackenzie’s review of the province’s largest care home outbreaks.
“There are these gaps. There has to be more oversight and more consistent standards,” said Cochlan, whose mother and father also lived at Lakeshore during their final days before they passed away just a few months apart in 2019 and 2020.
Her biggest frustration was the visiting rules, a concern that Mackenzie has also addressed.
VISITS TOO RESTRICTIVE
Cochlan believes that families should have had more opportunity to visit, with protocols for donning personal protective equipment, especially for those whose loved ones have dementia and may not be able to use FaceTime or understand what’s going on when the visit is short and the family member is two metres away.
“The essential visitors exemption should have allowed for regular visitors,” Cochlan said, noting that putting on full anti-virus protection “isn’t rocket science,” and something families would be very “motivated to do.”
“I was capable of doing it and was allowed to do it for two or three days for my mom (for end-of-life care), I’ll never understand why that wasn’t allowed for people with dementia, for whom six feet (apart) wouldn’t work.”
For months, Cochlan was the designated visitor, trying to get in as many visits as possible, signing up for extra days when there was room in the schedule.
Nash was used to daily visits so it was a hardship not to be with him every day.
“I know people must have died just because of the separation,” Cochlan said.
During the outbreak, visits were suspended and Cochlan had to wave and call to him outside his room. She counts herself lucky because he had a window.
However, when it appeared Nash was near the end from complications of COVID-19 Cochlan was declared an essential visitor. But when she saw him, he appeared to rally and even sang a bit of a jazz melody.
His improvement was short-lived.
The last time she saw Nash alive was through a window, while she stood outside the care home, on tip-toes, calling to him, hoping to catch a glimpse and maybe a snippet or two of song. Because he seemed to rally, she never expected him to go so soon, and when he did, she wasn’t there.
LASTING EFFECTS
Now that the outbreak has been declared over scheduled visits have resumed at Lakeshore and a magnolia tree will be planted for those who have passed away.
For Cochlan, the death of her husband ends six years of visits at the hospital — first for her parents, then her husband. It was a “close-knit” place, and impacts of COVID-19 will be long-felt by many, she said.
“They were just a very vulnerable population. Once the pandemic showed up, I know people did their best, it wasn’t for lack of good intentions,” she said, “But time will show the policies were maybe saving people’s bodies and not their spirits and their total wellbeing.”