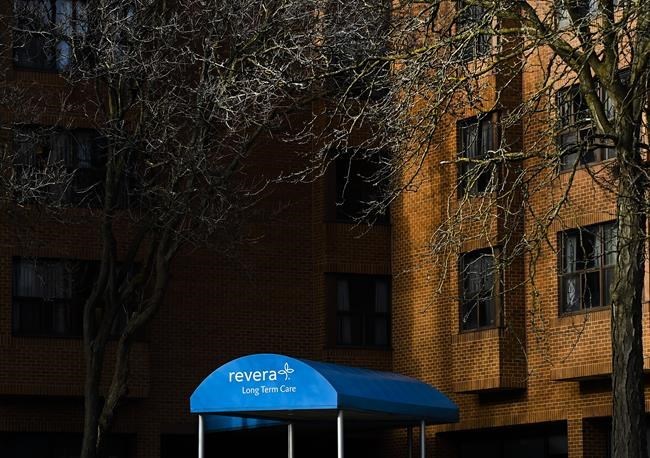
TORONTO — A new report from Revera Inc. calls out shortcomings in the public health system’s handling of the COVID-19 pandemic, even as the for-profit long-term care operator faces flak for its part in recent outbreaks.
Revera chief executive Thomas Wellner and panel chairman Bob Bell wrote that the report, titled “A Perfect Storm” and released Monday, is aimed at informing other operators in the long-term home sector, preventing future outbreaks, and restoring the confidence of workers and families in the long-term care sector.
Revera’s report, compiled by the 10-member panel of government, corporate and academic health care specialists, comes amid mounting concern about the for-profit long-term care sector in Canada. Revera is a for-profit enterprise owned by the Public Sector Pension Investment board, which is a Crown corporation that operates at arm’s length from the federal government. Revera has previously said it does not ask PSP for funding.
Critics of Revera including NDP Leader Jagmeet Singh have called for the government to transfer the company's facilities to public management.
A study published in the Canadian Medical Association Journal in August found the odds of an outbreak in for-profit homes like those run by Revera, were no greater than at non-profit residences. But the study also found that for-profit homes in Ontario were more likely to see more extensive COVID-19 outbreaks and a higher number of deaths.
After averaging an outbreak per day in Canada, the pandemic’s first wave resulted in 87 outbreaks at Revera residences, said the report, which covered events up to September. During that time, COVID-19 infected 874 residents and killed 266, a fatality rate of 30 per cent.
This autumn has brought new outbreaks to Revera homes as a second wave of infections sweeps the country.
The Revera report lobs several criticisms at government and public health officials that manage the sector at large.
Bell, for example, wrote in the report that he worried about a Revera manager who would have been devastated by the “thought of being unable to provide the best care for her residents – without provincial testing and without support from the barricaded health system surrounding her.”
“(Long-term) care in Canada is not a sector that can operate in a silo. Home operators – private, not-for-profit and municipal – must rely on critical investment, input and co-operation from across the health system to function well,” the report said. “COVID-19 not only exposed cracks within the sector, but also the broken links between it and the system as a whole.”
Revera said 97 per cent of its residents’ infections during the first wave of COVID-19 were linked to the period before April 13, because governments did not recommend masks for long-term care workers until early April and reserved masks and other protective equipment for hospitals.
The report covers up to September and does not track the source of infections for the ongoing wave of COVID-19, when masking protocols were already in place.
But it says that staffers' local communities were the main source of the first wave of infections after support workers, who make between $16 and $24 per hour, were banned from working at multiple sites for fear they would inadvertently “carry infection from one long term care home or retirement residence to another.”
Revera also said it needs more provinces to do COVID-19 testing every two weeks for all staff, not just during an outbreak. The report said local health authorities discouraged sending residents to testing sites.
“At one of Revera’s long term care homes, samples sent to a public health lab for testing were lost; in another case, test results were returned with confusing and incomplete information,” the report said. “(It) was not until early June that public health officials began visiting homes to provide regular testing to residents and staff in non-outbreak situations.”
The report also calls on governments to improve long-term care staffing, better train doctors on telemedicine, and speed up the approval process to modernize older homes — because that is where residents are more likely to share a room.
The report of nearly 100 pages concludes that Revera is already implementing many of the recommendations of the expert panel, which had “full editorial control” over the report and included several university-affiliated doctors or health policy experts.
However, Revera responded that some of the panel’s recommendations were aimed at “the broader system rather than Revera,” and that other recommendations couldn’t yet be fixed.
For example, Revera said it wasn’t yet feasible to follow the panel’s recommendations to move away from four-person rooms, hire full-time weekend nurses, free personal support workers from some reporting duties, staff a transitional wing for residents with COVID-19 cases, or lobby for immigration system changes to recruit more workers.
This report by The Canadian Press was first published Dec. 7, 2020.
Anita Balakrishnan, The Canadian Press